The most common skin conditions that present with chronic rashes on the face, trunk and limbs are due to seborrheic dermatitis, allergies, atopic and eczema. These skin conditions depending on the type and severity are treated with various medications including topical steroid creams, anti-inflammatory, immunosuppressant or antibiotics. Medications are most appropriately prescribed and be supervised by dermatologists.
Dermatitis refers to inflammation of the skin and can be classified in the following:
- Exogenous or contact dermatitis due to exposure to irritants, chemicals or cosmetics, causing allergies.
- Endogenous or constitutional eczema caused by changes in the body, hereditary or allergies.

Exogenous or Contact Dermatitis
The most common types are:
Irritant Contact Dermatitis
Irritant contact dermatitis is due to chemical exposure through home, work or pollution of natural environment. The exposure to chemicals can occur through the use of detergents and other highly-concentrated acid-based substances. Itchiness, redness or burning sensations are signs of exposure to these hazardous chemicals. These symptoms may subside, although allergies may be already formed.

Allergic Contact Dermatitis
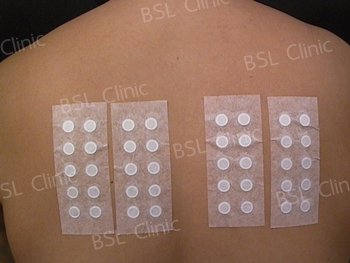
Allergic contact dermatitis is due to the exposure to substances that cause allergies. These substances include nickel, latex rubber gloves, shoe making materials and cosmetics containing fragrances and preservatives. If this happens immediately discontinue the use of these substances, which should help reduce the occurrence of the symptoms. These symptoms could persist for 1 to 2 weeks. The dermatologists will conduct a physical assessment and a patch test may be administered to determine the type of substances that cause the allergic reactions.


What is a patch test?
A patch test is a form of medical assessment that determines the types of substances that cause allergic reactions. These substances include nickel, latex rubber gloves, shoe making materials and cosmetics containing fragrances and preservatives. This test aims to confirm the specific substances that cause allergic reactions and as a way to reduce exposure, thus preventing further consequences. Completing a patch test can determine whether or not allergic reactions are caused from more than one substances to which the individual is exposed. The patch test cannot be conducted in pregnant women.
Endogenous or Constitutional Eczema
Endogenous or constitutional eczema is mainly hereditary. There are 2 major types of diseases within this group and they include both the atopic and seborrheic dermatitis.
1. Atopic Dermatitis (AD) – is a skin disease associated with asthma and pollen allergies. Patients present with high levels of Immunoglobulin E (found in people with allergies) are due to hereditary. The symptoms of AD are dry and flaky skin appearing on both cheeks and can spread to the neck and outer sleeves region.

Factors Causing AD Disease:
- Changes in weather conditions to being dry, hot or humid.
- Wearing clothes made from synthetic fibres or fur.
- Using soaps or ointments containing unnatural substances and preservatives causing irritation.
- Environmental pollution e.g. reduction in air quality and the built-up of dust or pollen.
- Stress and anxiety related issues.
- Products unsuitable for sensitive skin causing irritation.
- Excessive exposure to the natural elements e.g. sun and wind.

2. Seborrheic Dermatitis – is a symptom of skin disease which causes erythema or oily dry flakes on the top of the skin and white-yellow flakes that exfoliate. There are 3 body areas the symptoms regularly appear and these are included in the following:
- Face, nose, between the eyebrows, behind the ears and neck.
- Above the ribs, upper back, chest and armpits and scalp.
- In infants, it is found in the groin area, under the chest and navel.


Skin inflammation is the primary cause of an increased production of oily skin containing acidic substances and is found in people with seborrheic dermatitis. It is typically found in people within 3 age groups including infant after birth, young children and the elderly. Proper diagnosis should only be sought from specialised medical professionals, e.g. qualified dermatologists. The symptoms of seborrheic dermatitis are also associated with other diseases including Parkinson’s, neurological, malassezia infections and brain diseases.
Diagnosis – A BSL Clinic dermatologist will conduct an assessment to determine the family medical history of the patient.

Prevention and Treatment
Scalp Seborrheic Dermatitis
A shampoo product that is approved by the FDA is most suitable for use. Medicated shampoo is less effective due to its drug resistance. During shampooing, the product should be massaged into the scalp, left for 5 to 10 minutes before rinsing it off. This lets the substance absorb into the skin for effective results.
Seborrheic dermatitis, eczema or skin allergies are not treated with steroids. BSL Clinic’s preventative treatment does not involve thinning of the skin. This reduces the dandruff flakes that cause rashes.

Before Treatment – A 25-year-old man presents himself to BSL Clinic with chronic recalcitrant seborrheic dermatitis on the face and scalp. Both oral and systemic medication have failed to treat his skin conditions.

After Treatment – Effective results after 4 months.
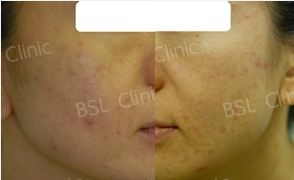
Before Treatment – The patient has received various treatments at other clinics with unsatisfactory results. Excessive sun exposure produces sensitive skin, red and papule in appearance.

After Treatment – The appearance of healthier skin is present due to the strengthening of the skin barrier. Skin sensitivity, rashes and redness disappear.

Skinesia Products – are created for patients with sensitive skin, sunlight allergies, itchiness, redness and rashes on their faces. It is most suitable for those who require special rehabilitation with 7 kinds of natural extracts to rejuvenate new skin cells. It reduces free radicals and oily skin when the individual is exposed to sunlight. These products do not contain steroids, dyes, fragrances, parabens, formaldehydes, alcohol or common irritants.
Article By
Dr Wipanee Akarapusit, M.D.
BSL Clinic Dermatologist